Abstract
Introduction
Anemia is a common complication of hematological chemotherapy for acute leukemia and following hematopoietic stem cell transplantation (HSCT). Exposure to allogeneic blood transfusions has been associated with unfavorable outcome in several studies in a non-surgical settings. Retrospective studies in hematological intensive unit have suggested that single red blood cell (RBC) unit transfusion policy may reduce the number of RBC used in comparison with a classical double RBC unit transfusion policy, without clinical impact. The aim of the study was to demonstrate that single RBC transfusion was non inferior to the standard double RBC transfusion arm in terms of severe complication or mortality for inpatient with hematological malignancies. Key secondary endpoint, was the comparison of the numbers of RBC units transfused in each arm.
Method
In a phase 3 multicenter randomized trial, 245 adults' patients with acute leukemia requiring intensive chemotherapy or patients receiving autologous or allogeneic HSCT were randomly assigned (1:1) to receive either single RBC unit (1 RBC arm, n=125) per transfusion or double RBC (2 RBC arm, n=120) per transfusion when hemoglobin level was below 8g/dL.
The primary composite endpoint was the percentage of patients who developed a grade ≥3 complications defined as stroke, transient ischemic attack, acute coronary syndrome, heart failure, elevated troponin level, intensive care unit transfer, death, new pulmonary infiltrates, and/or transfusion-related infections during hospital stays. The secondary endpoint was the number of red cell units transfused per patient per hospital stay. The primary endpoint was compared between groups by non-inferiority analysis for the proportion risk difference using Farrington-Manning method with a non-inferiority margin of 0.1, in ITT dataset.
Results
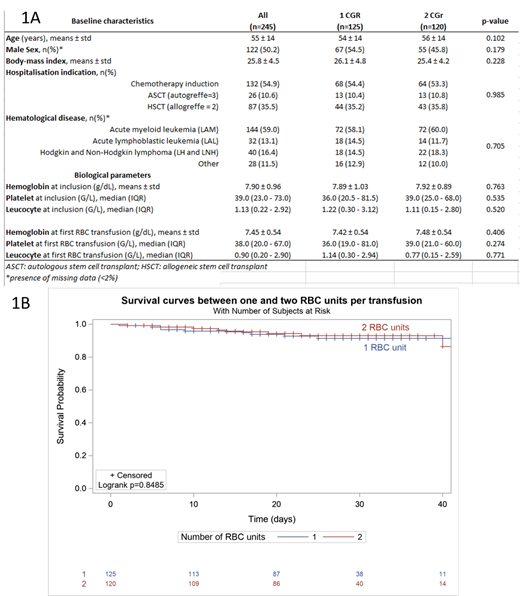
Hematological disease were as followed: AML (59%), ALL (13.1%), Lymphoma (16.4%), others (11.5%). The median age was 55 years. Baseline characteristics were well balanced between the 2 arms (Figure 1A). A total of 981 and 592 transfusions have been necessary in the 1 RBC arm and 2 RBC arm, respectively. The median of RBC unit per transfusion was 1(1-1) and 2(2-2) in the 1 RBC and 2 RBC arm, respectively. The mean pre transfusion hemoglobin level was 7.49 +/- 0.83 g/dL in the 1 RBC arm and 7.46 +/- 0.67 g/dL in the 2 RBC arm (p=0.275). Hemoglobin level at discharge was 9.35 +/-1.14 g/dL in the 1 RBC arm and 9.58 +/-1.13 g/dL in the 2 RBC arm (p=0.118).
The median (IQR) of red-cell units transfused per patient was 7 (4-12) in the single arm and 8 (4-12) in the double arm (p=0.65). The median number of platelet transfusion event was 7 (3.5-11.5) in the 1 RBC arm and 7 (3-13) in the 2 RBC arm (p=0.69). The median (IQR) number of red cell unit transfused per cycle and per day was 7 (3-9) and 0.28 (0.17-0.37) in the 1RBC arm and 6 (4-10) and 0.27 (0.20-0.38) in the 2 RBC arm (p=0.61 and p=0.47).
The predefined non-inferiority criteria was achieved with 28 patients developing a serious complication in the 1 CGR arm (22.4%) and 28 patients in the 2 RBC arm (23.3%) (Risk difference 0.009; 95% Confidence interval [-0.0791- 0.0978] (Figure 1B).
Conclusion: Single RBC transfusion policy is non inferior to double RBC transfusion policy in hematological intensive care unit for patient receiving a bone marrow transplant or intensive chemotherapy. Single RBC unit transfusion can be used safely in daily clinical practice. The single RBC transfusion policy does not reduce the number of RBC transfusion.
Jardin: Genexpath: Patents & Royalties: The author is a potential inventor on a patent application for the LymphoSign, which has been licensed for by Genexpath Patents & Royalties. .

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal